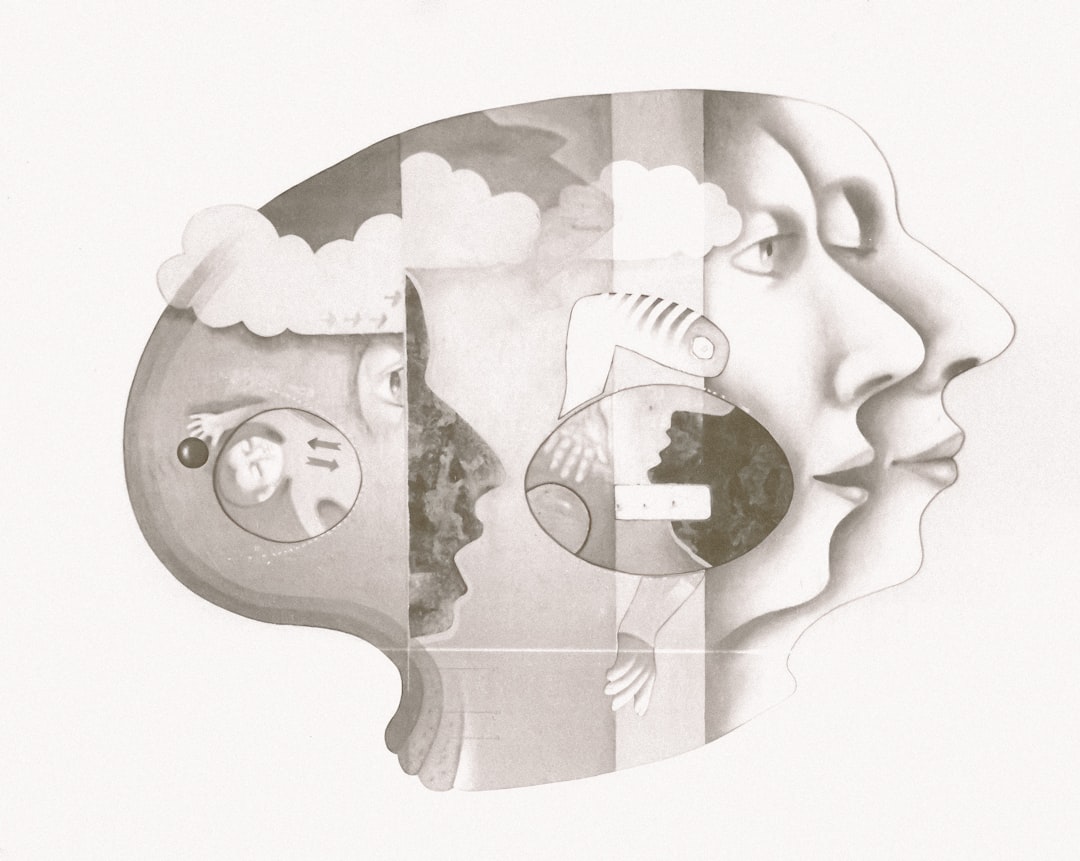
Trauma and the nervous system: understanding fight, flight, freeze and fawn

Trauma reshapes the nervous system in ways that can feel invisible and overwhelming. Je will guide you through the biology behind reactions like fight, flight, freeze and fawn, explain why hypervigilance and flashbacks occur, and outline trauma-informed therapy and practical stabilisation strategies that restore safety and regulation. I address this with clarity, warmth and clinically grounded language so vous can make sense of symptoms and options.
How the Nervous System Responds to Threat
The autonomic nervous system: a quick map
The autonomic nervous system (ANS) has two main branches: the sympathetic (mobilization) and the parasympathetic (rest-and-digest). When danger is perceived, the sympathetic branch activates adrenaline and cortisol, priming muscles and senses. The parasympathetic branch, especially the ventral vagal pathway, helps you reconnect, calm down and process safety signals. After trauma, this balance can shift, making threat responses easier to trigger and slower to settle.
The role of the brain in encoding threat
The amygdala, hippocampus and prefrontal cortex form a triad that manages fear, memory and regulation. Trauma can strengthen amygdala reactivity (heightened alarm), impair hippocampal context-setting (fragmented memories), and weaken prefrontal control (less inhibition of fear). This neural reshaping explains why benign cues sometimes feel perilous.
Understanding Fight, Flight, Freeze and Fawn
Fight and flight: mobilized survival strategies
Fight and flight are active responses: anger, confrontation, fleeing or frantic escape. Physiologically, heart rate rises, breathing becomes rapid, muscles tense. These responses are adaptive in acute danger but become problematic when they persist in safe contexts. Vous might notice sudden anger outbursts or panic even when no present threat exists.
Freeze and fawn: immobilization and appeasement
Freeze involves dissociation, numbness, or the feeling of being stuck. Fawn is a relational survival strategy: automatic people-pleasing or submission to avoid harm. Both manifest when escape or defense seems impossible. The body conserves energy; the mind reduces sensation. These patterns are subtle but deeply rooted in the nervous system’s attempts to preserve life.
Hypervigilance and Flashbacks: Memory Meets Sensation
Hypervigilance: scanning for danger continuously
Hypervigilance is an over-tuned threat detection system. It feels like never being able to relax, always scanning for signs of harm. Physiologically, baseline arousal stays high—sleep is disrupted, concentration falters. Cognitive load increases, leaving less bandwidth for work and relationships.
Flashbacks: when memory becomes present reality
Flashbacks are sensory-rich intrusions where past trauma feels current. They arise when the hippocampus cannot properly store contextual aspects of the memory, so cues trigger raw sensory-emotional fragments. Flashbacks can include smell, touch, visual fragments, and intense bodily responses. Grounding techniques and stabilization help interrupt this reliving.
Trauma-Informed Therapy: Principles and Practical Approaches
Key principles of trauma-informed care
Trauma-informed therapy prioritises safety, prediction, choice, and collaboration. Therapists validate experiences, avoid re-traumatization, and tailor pacing to the nervous system’s readiness. The aim is not to rush processing but to build capacity for regulation first.
Therapeutic modalities that work with the nervous system
Evidence-based approaches include Cognitive Behavioral Therapy (CBT) adaptations, Eye Movement Desensitization and Reprocessing (EMDR), Sensorimotor Psychotherapy, Somatic Experiencing, and pharmacological support when needed. Each addresses different layers: cognitive appraisal, memory reconsolidation, bodily regulation, and neurochemistry. I often emphasize combining stabilization with trauma processing for safe progress.
Stabilisation: Practical Tools to Regulate the Nervous System
Short-term grounding techniques you can try
Grounding anchors you in the present. Simple methods: 5-4-3-2-1 sensory check (name 5 things you see, 4 you can touch…), slow diaphragmatic breathing, splashing water on the face, or using weighted objects. These interrupt runaway arousal and bring back a sense of control.
Building long-term regulation and resilience
Regular practices grow nervous system resilience. Polyvagal-informed activities—safe social engagement, paced breathing, movement, and mindfulness—strengthen the ventral vagal pathway. Establishing routine sleep, nutrition, and gentle exercise stabilises baseline arousal and supports therapy work.
When to seek professional help
If symptoms significantly disrupt daily life—persistent hypervigilance, incapacitating flashbacks, chronic dissociation or self-harm—professional assessment is necessary. Trauma-informed clinicians will prioritise stabilisation, safety planning, and an individualised phased approach to processing.
- Trauma responses are rooted in nervous system adaptations, not moral failure.
- Fight, flight, freeze and fawn reflect adaptive survival strategies.
- Hypervigilance and flashbacks come from altered threat processing and memory encoding.
- Trauma-informed therapy pairs stabilisation with safe, paced processing.
- Practical grounding and lifestyle practices rebuild regulation over time.
Final summary: Making Sense of Trauma Responses and Recovery
I hope this overview clarifies how trauma reshapes the body and brain, and why symptoms like hypervigilance and flashbacks feel so convincing. Recovery is gradual. You can cultivate safety in the body through targeted stabilisation, informed therapeutic choices, and compassionate support. Avec patience and consistent practice, the nervous system can rebalance, and you can reclaim greater peace, presence and agency.
For clinicians or people seeking concrete examples of UK-based, trauma-informed services and practical stabilisation resources, see psychological-therapies-unit.co.uk for an outline of approaches that align with the methods discussed here.